
Philippine Pediatric Society, Inc.
A Specialty Division of the Philippine Medical Association (PMA)

This position paper was prepared by the Philippine Pediatric Society (PPS) Committee on Nutrition and its component society,
the Philippine Society for Pediatric Gastroenterology Hepatology and Nutrition (PSPGHAN)
This position paper was prepared by the Philippine Pediatric Society (PPS) Committee on Nutrition and its component society, the Philippine Society for Pediatric Gastroenterology Hepatology and Nutrition (PSPGHAN)
The First 1,000 days is the period that covers conception until the child reaches 2 years of age. It is a critical window of opportunities and outcomes.
Nutritional damage that occurs during this period is irreversible.
A decrease in the national prevalence of stunting (being short for age) is now the preferred indicator for measuring outcomes in nutritional interventions.
There are nutrition-specific interventions that have been proven to work. The challenge is to integrate, accelerate and sustain actions.
There are nutrition-sensitive interventions that may need to be prioritized by the government. These include agriculture, social welfare and education.
The Philippine Pediatric Society is part of these solutions. It is a credible messenger that can help focus on interventions that work.
In 2008, The Lancet medical journal published a series of papers on maternal and child undernutrition. These papers identified a critical window of time between a womans pregnancy and her childs second birthday, which was later coined The First 1,000 days.
The First 1000 days is a period when a child has increased nutritional needs to support rapid physical growth and mental development. This is also a period when the mother and her child are most at risk of malnutrition and infections. It has been shown that growth faltering of the child begins in the mothers womb and continues until the child reaches 2 years of age. Children born with low birthweights (<2,500 grams) due to restricted growth inside their mothers wombs are at great risk of remaining stunted. This early chronic exposure to inadequate nutrition is captured by one important anthropometric indicator- stunting (inadequate length/height for age).Any loss in linear growth during this period is not recovered later in life and catch up growth is minimal
Lack of adequate nutrients during this period of rapid brain development has long-term effects on cognition which are not recovered even with improvements in nutrition after 2 years of age. The outcome of brain development by the age of two years determines to a large extent a persons mental capacity for the rest of his/her life, including success in schooling and income earning.
Data from the 2013 National Demographic and Health Survey show that the prevalence of nutritionally at risk pregnant women in the country due to being underweight is 24.8%with the percentage of low birth weight babies being born in the country increasing from 21% in 2008 to 23.2% in 2013.
The Philippines ranks 9th in terms of the number of children under 5 years old who are moderately or severely stunted. Although the national prevalence of stunting is about 33%,(3 out of 10) there are pocket areas wherein there is still a high magnitude and severity of stunting at ?40% (4 out of 10). These are MIMAROPA, Bicol region, SOCCSKSARGEN and Autonomous Region in Muslim Mindanao.
The right nutrition delivered at the right time within this 1,000-day window can have a profound impact on a childs ability to grow, learn and rise out of poverty. Children who get the right nutrition in their first 1,000 days are 10x more likely to overcome the most life-threatening childhood diseases. They complete 4.6x more grades of school. They go on to earn 21% more in wages as adults. More importantly, they are more likely as adults to have healthier families.
The Philippine Pediatric Society fully supports a programming focus of the government to this 1000-day period from conception up to 2 years of age.
The Solution
Simple solutions that focus on the first 1,000 days already exist. There is a need to focus on integrating and accelerating these evidence-based actions at scale and sustaining all initiatives.
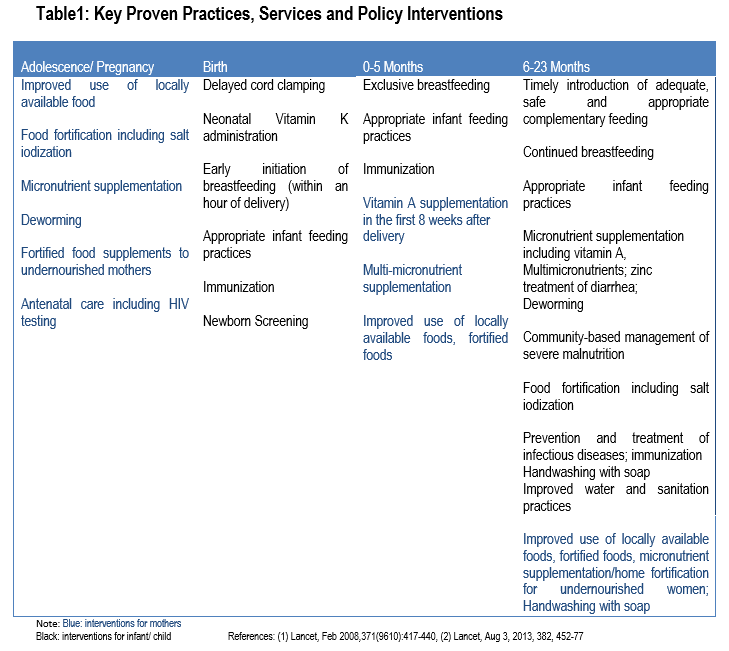
Evidence-supported interventions that address very specific requirements of adolescent girls, pregnant women, mothers and their children have been identified (Table 1). These are referred to as nutrition-specific interventions.
A. Interventions for women of reproductive age (WRA) (for midwives ,obstetricians and other
birth attendants)
a. Iron-folate supplementation including adolescent girls. Adolescence is defined as between
10-19 years old (World Health Organization definition).
b. Multimicronutrients supplement with iron-folate-calcium for all pregnant women
c. Maternal supplementation with balanced energy and protein including education and counselling
on proper nutrition
d. Vitamin A supplementation within the first 8 weeks post-delivery (200,000 IU single dose)
e. Salt iodization or use of iodized salt
f. Focused antenatal care which involves a minimum of 4 visits in normal or uncomplicated
pregnancies must be encouraged
i. 1st visit: before 4 months
ii. 2nd visit: 6 months
iii. 3rd visit: 8 months
iv. 4th visit: 9 months
Note: For pregnant women with possible or expected complications, prenatal visits may be more frequent depending on the recommendation of the attending health personnel.
g. Components of Focused Antenatal Care
1. QUICK CHECK for emergency signs for which an immediate referral to the nearest hospital is
recommended:
a. Vaginal bleeding
b. Severe abdominal pain
c. Looks very ill
d. Severe headache with visual disturbance
e. Severe difficulty of breathing
f. Fever
g. Severe vomiting
h. Unconscious/convulsing
2. Registration and issuance of a mother and child record/ home based record.
3. Assessment:
First visit:
a. Medical history: age, past medical history
b. Obstetric history: last menstrual period, age of gestation, gravidity
c. Prior Pregnancy (second time mothers)
i. Presence of convulsions
ii. Stillbirth or death
iii. Heavy bleeding during or after delivery
iv. Prior cesarian section, forceps or abortion
d. Baseline haemoglobin, blood type, urinalysis. If haemoglobin is <8g/dl, refer to an
obstetrician for work up and treatment of anemia. Check urine for the presence of protein.
e. Screening for diseases that may complicate pregnancy.
i. Ask about family history (first degree) of diabetes and history of obesity; Previous pregnancy for difficult labor, large babies, congenital malformations and previous unexplained fetal death
ii. Look for signs of maternal overweight and obesity, polyhydramnios, signs of large baby or fetal abnormality, vaginal infection
iii. Refer for glucose test: at 24-28 weeks for low risk or immediately if high risk.
iv. Check for fever, burning sensation and abnormal vaginal discharge. Ask about episodes of fever or chills and take temperature. Ask about pain or burning sensation on urination. Ask about presence of abnormal vaginal discharge, itching at the vulva or if partner has urinary problems.
f. Preventive measures: Immunize against tetanus (to be provided by the RHU)
Tetanus toxoid at least 2 doses: the first dose at first contact with the woman or at first antenatal visit and the last dose must be given at least 2 weeks before delivery.
g. Discussion of a birth and emergency plan
i. A birth plan is a written document prepared during the first antenatal visit. This may change anytime during pregnancy if complications develop. It contains information on: the womans condition during pregnancy, preferred place of delivery and choice of birth attendant, available resources such as transportation, companion and money for her childbirth and newborn baby, preparations needed such as blood donor, referral center should an emergency situation arise during pregnancy, childbirth or postpartum
ii. An emergency plan includes information on danger signs, signs of labor, where to go, how to go, what to bring, with whom to go, who will care for the home and the first child when she is away.
On all visits:
a. Check duration of pregnancy (AOG)
b. Ask for bleeding/danger signs during pregnancy
c. Check record for previous treatments received during this pregnancy
d. Prepare birth and emergency plan
e. Ask patient if she has concerns
f. Give education and counselling on family planning.
g. Check for hypertension. If BP is above 140-90 early in pregnancy, referral to a doctor is made. If diastolic BP is 90 mmHg or higher, repeat measurement after 1 hour rest. If diastolic BP is still 90 mmHg or higher, ask the woman if she has 1)severe headache 2) blurred vision 3) epigastric pain
If urine has protein: and all the above are present, referral for possible pre-eclampsia should be made.
B. Interventions in neonates
a. Delayed cord clamping
i. Delayed cord clamping is approximately 1-3 minutes after birth (NOT
b. Neonatal Vitamin K administration
i. One dose of intramuscular vitamin K after birth will reduce clinical bleeding at 1-7 days of life including bleeding after circumcision.
ii. Term babies 1 mg IM soon after birth
iii. Preterm babies <1000g, 0.5 mg IM soon after birth
iv. Dose of oral vitamin K if intramuscular vitamin K cannot be given i.e. home births and refusal of parent or if with no health care worker who could administer, 3 separate doses need to be given as follows:
o 2 mg oral soon after birth
o 2mg oral at 3-7 days
o 2mg oral at 6 weeks
c. Kangaroo mother care for promotion of breastfeeding and care of preterm and small for gestational age (SGA) infants. It has 3 parts namely,
i. Skin-to-skin contact at birth and even short periods during day or night
ii. Exclusive breastfeeding
iii. Support to the dyad- medical, emotional, psychological support
d. Newborn Screening
e. Immunization
i. BCG vaccine, single dose given at birth
ii. Hepatitis B vaccine given at birth
C. Interventions in Infants and Children
i. Promotion interventions and counselling on breastfeeding
ii. Promotion of dietary diversity from 6 months to 23 months of age
a. Provision of nutrition education
b. Provision of additional complementary food.
iii. Vitamin A supplementation
a. Vitamin A can reduce all-cause mortality by 24% and diarrhea-related mortality by 28% in children 6-59 months. It can also reduce the incidence of diarrhea and measles in this age group.
| Title | |||
|---|---|---|---|
| PPS PIDSP Position on Vaccination in Children (09 August 2021) |
Download | ||
| Care of the Newborns during Covid-19 Pandemic (PSNbM) (30 July 2021) |
Download | ||
| FAQs on COVID-19 IgM/IgG RAPID DIAGNOSTIC TESTS (01 April 2020) |
Download | ||
| PPS/PIDSP Interim Guidelines on The Screening, Assessment And Clinical Management of Pediatric Patients With Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) (30 March 2020) |
Download | ||
| VACCINATION DURING THE COVID-19 PANDEMIC: PPS and PIDSP RECOMMENDATIONS (29 March 2020) |
Download | ||
| Information on COVID-19 for Clinicians: Additional Guidelines for Outpatient Pediatric Care in the Philippine Setting from the Philippine Pediatric Society and the Pediatric Infectious Disease Society of the Philippines (10 March 2020) |
Download | ||
| Support the DOH Vaccination Campaign Against Polio: An Urgent Appeal to the Pediatricians from the Philippine Pediatric Society and the Pediatric Infectious Disease Society of the Philippines (15 February 2020) |
Download | ||
| Frequently Asked Question on Poliovirus Immunization for Pediatricians (28 October 2019) |
Download | ||
| Detection of a Polio Case Announced by DOH: Guidance for Clinicians (19 September 2019) |
Download | ||
| Statement of Support for the Department of Health Polio Supplemental Immunization Activity (29 August 2019) | Download | ||
| First 1000 Days | Download | ||
| On the Minimum Age of Criminality | Download | ||
| The Minimum Age of Criminal Responsibility Act | Download | ||
| The Unmitigated Killings of Suspected Drug Users that have Affected our Children, Adolescents, and their Families, and the Random Drug Testing of School Children. | Download | ||
| Japanese Encephalitis Vaccines | Download | ||
| Hepatitis B Birth Dose Multisectoral | Download | ||
| HSP Position Statement on Hepatitis B Vaccination | Download | ||
| Statement on the use of the Dengue Vaccine (May 20, 2016) |
Download | ||
.
Christmas time.
Through the years we have defined and described this season so many ways. We have created this time of the year as a joyous and festive celebration. That is of course true, for there is no greater joy than the day the Savior was born. It is of course a season to celebrate because the Salvation of man and its story will now come into fruition.
But just like how different individuals are, Christmas is also observed in the hearts of men differently. Some enjoy Christmas for the avalanche of gifts. Some are just thankful for being alive. Some muse because of the variety of food to eat. Some just say a prayer to continue to survive. But there is a unifying factor in why Christmas is special it is the coming of the child who will make every man equal in the story of salvation.
No matter what sweeps our hearts in this season of Christs birth, we have a lot to be thankful for.
The PPS has a lot to be thankful for.
We remain a resilient Society. A group of people called upon to help deliver healthcare services to the young and tasked to preserve a future they all deserve.
We remain a strong Society. A group of professionals who when called to action go beyond their duties and take the extra mile to do their best in everything they have put their minds into.
We remain a courageous Society. A group of determined professionals who take principles positions on issues that require both conviction and competence.
We remain a determined Society. A group of specialized doctors who weathered the resurgence of diseases in outbreak proportions measles, dengue and now polio. We rally behind the government in its earnest efforts to curb the spread of these diseases protecting every child to the best of our abilities.
Christmas is a time of hope. A time to look beyond what is here. A time to aspire for a better future.
Christmas is a time of love. A time to share what we have been blessed. A time to wish others the blessings they deserve.
Christmas is a time of peace. A time to pray for each others solace. A time to bring happiness to every single man we can.
Some find joy in Christmas because it reminds them of their youths. Some shed tears during Christmas because it witnessed the loss of people and properties they once cared for. Some find exuberance during Christmas because the sight, the sound and the smell of the cool breeze brings them unspeakable happiness. Some find sadness in Christmas because of the indifference and confusion the occasion brings.
No matter what makes us happy or sad in this season of Nativity, we have a lot to look forward to.
The PPS has a lot to look forward to.
We remain a formidable Society. A group of experts who know what they are doing and who are willing to teach others how to do it well.
We remain a vibrant Society. A group of colorful individuals coming from all spectrum of the human form, bearing individuality that spells diversity and welcoming everyone with an inclusivity that knows no distinction.
We remain a vigilant Society. A group of dedicated physicians who look after each other, who put the interest of the Filipino child above self and who respects the ideals for which the PPS was envisioned and established.
And as we join our families a few days from now to be one in the celebration of Christmas, let us not forget to find Christ in this season because He is the reason and He is the season itself.
It is only in finding Christ in the letters of the word Christmas can living be appreciated as a precious gift, that prayers answered or not are heard, that tears of loss have the promise of joy and that sadness will one day be rewarded with genuine happiness.
Merry Christmas to all of you.
Delivered by the PPS President , Salvacion R. Gatchalian , MD , during the Annual Christmas Party of the Philippine Pediatric Society December 11, 2019 at Novotel Manila Araneta City.
The Philippine Pediatric Society, true to its commitment in ensuring continuing medical education for all its members from all over the Philippines, will be introducing the Continuing Professional Development Online (CPD Online).
CPD Online is designed to foster and maintain a high plane of skills in the practice of Pediatrics. It will focus on topics that are relevant to Pediatric Medicine; advance knowledge, skills and / or ethics; and be delivered by certified pediatricians or experts in related medical fields.
Member participants to this course will earn one (1) unit for every completed CPD Online activity. This will complement 30% of your annual CPD requirements at the very comfort of your clinics or homes at your most convenient time. This is certainly good news to everyone!
Dear Colleague,
Greetings! I am the Principal Investigator of a research project entitled Nationwide yaws active surveillance and case detection in selected areas of Luzon and Visayas regions in the Philippines, in cooperation with the Department of Health (Infectious Diseases Office Disease Prevention and Control Bureau and Health Policy Development and Planning Bureau) and the Philippine Council for Health Research and Development (PCHRD). The implementing agency is the Philippine Leprosy Mission, Inc. Its main objective is to determine the presence of at least one active or latent yaws case in each of the regions of Luzon and Visayas. The presence of at least one case in a locality makes it endemic for yaws.
Yaws is non-venereal treponemal infection mainly affecting the skin and the bones in children. It is one of the Neglected Tropical Diseases that is potentially eradicable. There have been confirmed active yaws cases in Mindanao detected in 2017 during a study conducted by this Investigator. Due to this pioneering study, the World Health Organization has recognized the Philippines as the 14th country endemic for yaws.
This second yaws study is conducting an active surveillance system so that we can pick up reports from health professionals including members of the Philippine Pediatric Society. This project entails the following activities:
1. Through email, you will be given information on yaws and instructed to familiarize yourselves with the clinical characteristics of yaws.
2. You will be invited to answer an online questionnaire about yaws even if you have never encountered yaws in the past. Informed consent will be secured.
3. You will be requested and reminded to refer any yaws suspects to the Principal Investigator anytime during the study period until May 2020.
Please extend your cooperation and assistance for the successful implementation of this study by accomplishing the Google Form within 2 weeks of receiving it. Please click on the link
https://forms.gle/FVeW44Kp6h91FNwC7
If you accomplish and submit the online questionnaire, you will have a chance to win a token prize during a raffle at the end of the study period.
Attached are the Yaws information materials (Yaws Fact Sheet, Yaws Recognition Booklet, Yaws Clinical Photos of Filipinos) for your perusal before answering the online form.
If you have any questions regarding the yaws study, you may contact me at 0917-6294329 or belendofitas@gmail.com. Thank you for your valuable support!
Sincerely yours,
BELEN L. DOFITAS, MD FPDS
Principal Investigator
Yaws Study II
Downloads:
Letter YawsII PPS member Aug10 2019
Yaws ClinicalPhotos Filipinos
YAWS FACT SHEET WHO may 21 2019
YawsRecognitionManual